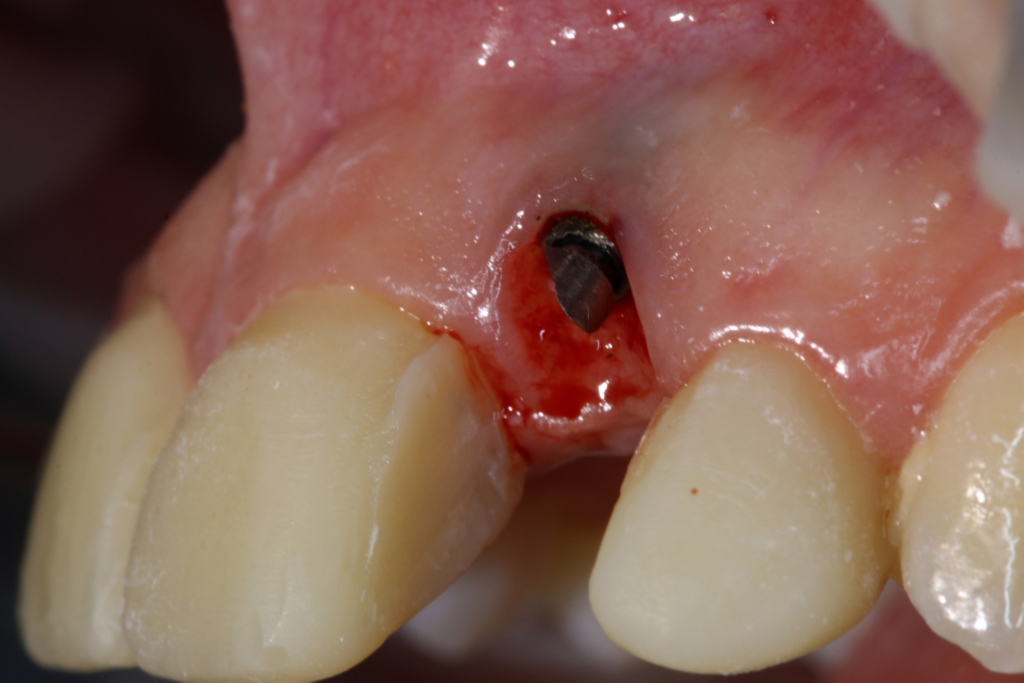
Kristin was recently seen by a dentist who placed a dental implant to replace one of the front teeth. Can you tell which tooth is the Dental Implant?

Unfortunately for her, you probably can. She was very unhappy with the cosmetic result of that terribly long tooth, and sought out Dr. Zidile’s expertise to correct the problem. Here’s a close up – note the artificial, grey gum appearance. A final case photo will be posted soon!
Long term Implant complications, or Peri-implant diseases, are inflammatory conditions affecting the soft and hard gum tissues around dental implants. Similar to a natural tooth, bacteria can build up on the base of the implant, below the gum line. Just like your natural teeth, implants require regular tooth brushing and flossing and regular check-ups from a dental professional – and a periodontist is best suited to diagnose and treat this condition. If you have a dental implant in your mouth, you should have it examined on an annual basis.
See article below from The Telegraph in the UK.
By Ruth Wood
July 14, 2014
Cathy Gunnell was thrilled when she had dental implants fitted at the age of 52. Since childhood, she’d endured crooked teeth, gum disease and abscesses, one of which forced her to have a tooth removed.
So when a local London clinic charged her £13,000 to replace four diseased teeth with gleaming white porcelain ones, fixed in place with metal pegs, she was more than happy to pay.
That was in 2002, and for 12 years she had no problems. But three months ago, she felt a lump on her lower right jaw near one implant. “There was no pain, but I got it checked out by my local dentist,” says Mrs Gunnell, now 64.
The lump was caused by inflammation that cleared up after antibiotics. But an X-ray showed the bone supporting the implant was receding.
To her shock, Mrs Gunnell’s dentist diagnosed her with a little-known disease that is now emerging as a serious complication of dental implants. It is called peri-implantitis, and has been described as a “time bomb” by a leading dental surgeon.
Peri-implantitis is an inflammatory disease marked by bacterial infection and the gradual loss of the jaw bone supporting the implant. It’s not yet clear whether the infection causes the bone to recede, or the bone loss exposes the area to bacteria. Dentists are uncertain how to treat it. “I was shocked,” says Mrs Gunnell. “I’d never heard of the disease.”
Ten years ago, professionals said the condition didn’t exist. But now it is on the rise, as increasing numbers of people have replacement porcelain crowns with titanium roots. Half-a-million adults have at least one dental implant, according to the latest Adult Dental Health Survey.
Studies have suggested that one third of patients will be infected. “We’re sitting on a time bomb,” says Dr Stephen Jacobs, a past president of the Association of Dental Implantology and well-respected implant surgeon. “We are going to be seeing more and more cases.”
Peri-implantitis is always preceded by a much milder disease, called peri-implant mucositis, which is common and treatable. Early warning signs are red, swollen gums and bleeding when probed. If undetected and untreated, it might become peri-implantitis.
Because bone loss is painless, many people don’t realise they have the condition. So scrupulous oral hygiene and regular follow-up appointments after an implant are essential, says Dr Jacobs, who runs a Glasgow clinic. “One of the problems with seeking treatment abroad [as many do in search of cheaper treatment] is the lack of lifelong maintenance and follow-up, which is a key part of the care process.”
Mrs Gunnell stopped going for check-ups three years ago, after she moved from London to Devon. She was at high risk of peri-implantitis because of a family history of gum disease (periodontitis). Smokers, too, are at high risk.
Paradoxically, the rise in cases is mostly due to advances in implant design. In the mid-Nineties, clinicians found that implants with a rough instead of a smooth surface integrated better with the bone. However, the textured surface is more likely to harbour bacteria if the bone shrinks away from it.
After her recent diagnosis, Mrs Gunnell returned to the London prosthodontist who originally treated her. “He removed the bridge and screws and deep-cleaned the whole area and all the components,” she says. “He told me to brush with TePe brushes [small interdental brushes] dipped in Corsodyl [antiseptic mouthwash], morning and night, and to come back for yearly check-ups. Hopefully that will keep the infection at bay. I hope so, because I’ve made such an investment in my teeth.”